Dr Maria Pecsek MD
The beginner Basal Cell Carcinoma is a precancerous state therefore it is risky and dangerous.
The precancerous state can very quickly turn into a cancer if it is not treated in the early phase.
The solution is immediate treatment. Do not wait! Start the treatment in your home with the R47-PROTUMOL® treatment cream.
R47-PROTUMOL® treatment cream benefits
Clinically tested ● No prescription required ● Not a medicine ● Quick and efficient ● Zeros side effects ● Safe ● Contains solely vegetable active ingredients ● Zero hospital intervention ● Zero doctor’s assistance ● Can be applied at home at work and in leisure time ● Anyone can use it at any age ● Simple to use ● It can be applied on the whole surface of the body ● No need to cover the surface after applying the cream ● The cream is non-sticky ● Absorbs quickly, like a face cream ● It leaves no stain on clothes ● It doesn’t have an unpleasant smell

J. Seguin
Paris – France
A dermatologist diagnosed a basal cell carcinoma on my back one year ago. The doctor said that before the operation I should try out a cream and I may not need the operation. I used R47-PROTUMOL® cream three times a day. The basal cell carcinoma started to nicely shrink and it was completely gone in 5 months. I didn’t need the operation.
M. Bertrand
Marseilles- France
I am a sailor so I am exposed to a lot of solar radiation. As a result of the sunlight a mole on my shoulder turned into a malignant basal cell carcinoma. From my colleagues I heard about R47-PROTUMOL® cream and how effective it was against skin cancer. I started to use it myself. It proved to be efficient very soon. Within three weeks the size of the tumor decreased by 50%. After six months only a faint spot remainds me of the tumor.
L. Siméon
Monte Carlo – Monaco
In Monaco the number of hours of sunshine is high all year round. A pea-sized wound formed on my forehead. After dermatological examination I was told that I had skin-cancer. I read in the Jet Set Côte d’Azur magazine how effective the R47-PROTUMOL® cream is against skin cancer and actinic keratosis. After a few months of treatment the cream eliminated the skin cancer on my forehead.
F. Maréchal
Nice – France
Actinic keratosis formed on my face as a result of strong solar radiation. Following my doctor’s recommendation I started to use the R47-PROTUMOL® cream. Within a relatively short period the actinic keratosis was gone. Because I spend a lot of time outdoors in the sunlight and my skin is sensitive I’ve since had actinic keratosis and basalioma on other parts of my body too. R47-PROTUMOL® cream provided me full support. I’ve never had to undergo any operation.
H. Fischer
Berlin – Germany
I had ulcerated basal cell carcinoma. The ulcer could not be eliminated with traditional treatments. As long as the tumor is ulcerated it cannot be operated. The situation got worse with every passing day. I had to find a solution because this ulcerated tumor can cause death. R47-PROTUMOL® cream was recommended to me by a patient in the hospital. I purchased it and started using it. After two weeks of treatment the ulcerated wound started to close down. After three months of using the cream the wound completely closed down and its size decreased from 3 centimeters to 4 millimeters. I returned to the hospital and the dermatologist said that it could be operated on. It was cut out, I am absolutely healthy but just in case I continue using the cream.
K. Ulrich
Hamburg – Germany
I had skin cancer. I treated the cancerous surface with R47-PROTUMOL® cream. The cream was so effective for me that even my doctor was surprised how fast it proved to be effective for me.
G. Klein
Vienna – Austria
I was diagnosed with basal cell carcinoma on my neck. I was operated on. After the operation the operation scar didn’t heal, I visited the doctor’s office almost every day. I learnt about R47-PROTUMOL® cream, I purchased one and I applied it on the skin twice a day. After approx. two weeks a thin pellicle formed on the wound, the exudation stopped, the diameter of the wound nicely decreased. For the first time after one and a half years I started to see some hope that I may recover. For the moment I use the cream once a week, only a light red spot reminds me of my wound.
F. Berger
Salzburg – Austria
So far I have been operated on for actinic keratosis four times. On every occasion this skin malformation formed on a different spot on my face. My dermatologist recommended treating my facial skin with the R47-PROTUMOL® cream for prevention. I followed the recommendation I have been using the cream for three years. Since then I haven’t had another actinic keratosis.
S. Steiner
Geneva – Switzerland
I had basalioma on my face. My French friends recommended the R47-PROTUMOL® cream. I applied the cream on the affected surface. Within one month the basal cell carcinoma started to heal, in three months it was completely gone.
A. Pliszeckaja
Moscow – Russia
My skin is very sensitive. So far I’ve had basal cell carcinoma on my face three times. Twice I had actinic keratosis on my shoulder. Altogether I’ve been operated on five times. In Monaco my husband gave me a copy of the Jet Set Côte d’Azur magazine. It was from this magazine that I got to know about R47-PROTUMOL® cream. After returning to Moscow we ordered the cream that I’ve been using ever since. I haven’t had another basal cell carcinoma or actinic keratosis even though I spend a lot of time at the sun. What’s more I find this cream to be more beneficial to my skin than any of the expensive face creams. The large amount of plant-based active agents and vitamins give a young look to the skin.
B. Belinszkij
Saint Petersburg– Russia
I got diagnosed with a malignant melanoma on my arm. I got very scared because I know that in 80% of the cases melanoma causes death. A friend of mine who is a diplomat in the EU brought me some R47-PROTUMOL® cream. After four months of using the cream I was symptom free. I’ve continued using the cream since then, I apply it at least once a day on the surface of the once existing melanoma.
M. Kralova
Kosice – Slovakia
I treated a basal cell carcinoma in the corner of my mouth with R47-PROTUMOL® cream. After two weeks the size of the skin cancer was so small that only a small spot could be seen. My doctor suggested that I should continue the treatment with the cream and I may not have to be operated on. I didn’t need the operation because the basal cell carcinoma completely vanished from the corner of my mouth. I am very grateful for the creators of this cream.
S. Zakar
Budapest – Hungary
I read about the R47-PROTUMOL® cream in a paper, telling how effective it is in treating skin cancer. It was a birthmark on my back which degenerated, and turned into a malignant melanoma, with a 2 cm diameter and a 1 cm height. 2 months ago I bought the cream, and my wife applied it on the surface of the melanoma twice a day. Presently, the diameter is less than 1 cm, and has no height, it completely subsided, as it became even with the normal skin surface. It is reducing day by day.
Sz. Kovács retired teacher
Budapest – Hungary
A pea-size lesion appeared on my forehead. I could not trace it back to any antecedent. After a dermatological examination I was told that I have melanoma skin cancer, and I need to be operated on. After the surgery the scar did not start healing, and I was visiting the doctor’s office almost every day. I got quite depressed as, it being a not too big scar, I undertook all prescribed therapy. I heard about the R47-PROTUMOL® treatment cream, I bought one, and applied it on the scar twice a day. It was after about two weeks that a thin film appeared on the scar, it stopped exuding juice, and its diameter also neatly reduced. It was the first time after one and a half years that I had a flash of hope that I might recover. For the time being I apply the cream once a week, and by now it is only a pale red spot that witnesses my scar.
K. Radnai
Győr – Hungary
An ulcerous tumour was removed from the ridge of the nose between the eyes. To my greatest surprise the scar did not heal. It exuded juice, then after 1-2 days a thin film developed, but then it got ulcerated again. I ordered a tube of the R47-PROTUMOL® cream to give it a try. I applied it on the above-mentioned scar daily. After a week the scar started to contract, exuding juice ceased, and the scar nicely healed. Now I am applying the cream only once a week.
F. Angyal
Budapest – Hungary
I am suffering from ulcerated melanoma skin cancer. It cannot be operated on. In “Zöld Újság” (Green Magazine) I read the letters of people suffering from similar diseases. I thought I myself will try using the R47-PROTUMOL® cream. The cancer appeared on the part behind the ear. I apply the cream on the surface twice a day, and healing process started within 10-11 days after I started to do so. The scar has healed over.




Trusted by Thousands of Happy Customers Since 2006
Here are some reviews from our customers from around the world.Hover on the markers on the map to see user reviews.
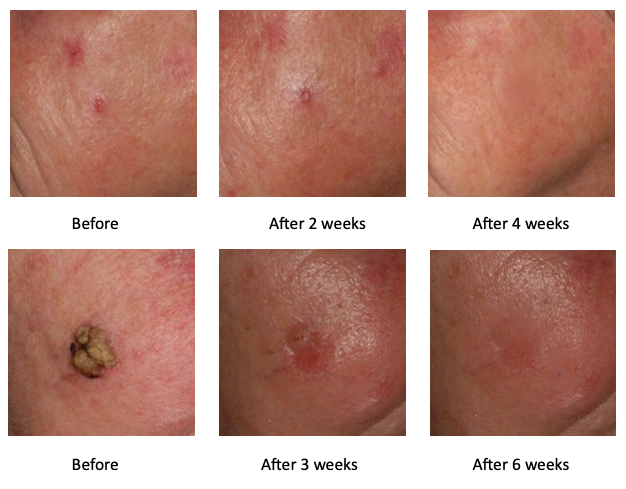
Of course, there may be individual differences from those shown here. Results may vary from individual to individual and are not guaranteed.
How to use the R47-PROTUMOL® treatment cream?
- For Skin cancer: Apply the Cream on the skin surface to be treated in a thin layer three times a day: in the morning, at noon, and in the evening.
- For Breast cancer: Apply the cream in a thin layer three times a day on both breasts and the armpits. It is recommended to apply the cream on both breasts and armpits even if the tumor is present only in one breast. The R47-PROTUMOL® cream is safe and effective in case of ulcerous tumor too.
- Note: Before each application wash the surface with ample water so that the layers of the cream don't stack up on each other. Washing the surface is necessary because layers of cream on top of each other block the absorption of the active ingredients.
It is not recommended to use the R47-PROTUMOL® treatment cream on the same skin surface simultaneously with other creams or body lotions or any other product of cutaneous use.
Qualities of the R47-PROTUMOL® treatment cream
The active ingredients of the cream consist of such different groups of ingredints that have anti-cancer and immune-system strengthening effects, such as e.g. antioxidants, several vitamins, minerals, carbohydrates, proteins, flavonoids, enzymes and organic acids.
- What characteristics do these materials have?
- Antioxidants defend the organism against the deleterious effects of the free radicals and so they slow down the aging of the cells, hold down the malignant degeneration of the cells, and support the immune system.
- Vitamins: the building blocks of our body, they defend the organism against the deleterious effects of the free radicals acting against the organism, thus slowing down the aging of the cells, holding down the malignant degeneration of the cells, and supporting the immune system.
- Flavonoids: they have an anti-cancer effect.
- Amino acids: they play a decisive role in building up the proteins.
- Proteins: indispensible constituents of all cells.
- Carbohydrates: their main physiological role is energy production.
- Enzymes: bio-catalysts of the processes going on in the human body.
- Minerals – their macro and micro elements, which are so called elements providing vitality, play an important role in the smooth functioning of the organism.
- Trace elements, which strengthen the organism, help recovering from illnesses, and are of help against the development of tumorous diseases.
Dr Maria Pecsek MD: Why do I use the R47-PROTUMOL® treatment cream in my medical practice? Because this cream is first aid for the skin! Quick and efficient. No side effects.
Facts:
- More than 940 million people worldwide suffer from Basal cell carcinoma and Squamous cell carcinoma.
- According to one estimate, about 8.2 million basal cell carcinoma are diagnosed each year in the US.
- According to a report by the WHO, the number of skin tumor patients will double by 2040.
What is the solution?
- The goal is to provide risk-free treatment for Basal cell carcinoma and quickly reach the symptom-free stage! This is the most important thing for skin problem sufferers. Their expectation is that the treatment is comfortable, free from side-effects, has rapid impact so that the treatment can have a positive result even within a few weeks.
- The clinically tested R47-PROTUMOL® treatment cream may be applied on its own but also as a complement to medicine therapy. This product is not a medicine and it is available without a prescription.
Quick and efficient. No side-effects.

About Basal cell carcinoma
Basal cell carcinoma is a type of skin cancer. Basal cell carcinoma begins in the basal cells — a type of cell within the skin that produces new skin cells as old ones die off.
Basal cell carcinoma often appears as a slightly transparent bump on the skin, though it can take other forms. Basal cell carcinoma occurs most often on areas of the skin that are exposed to the sun, such as your head and neck.
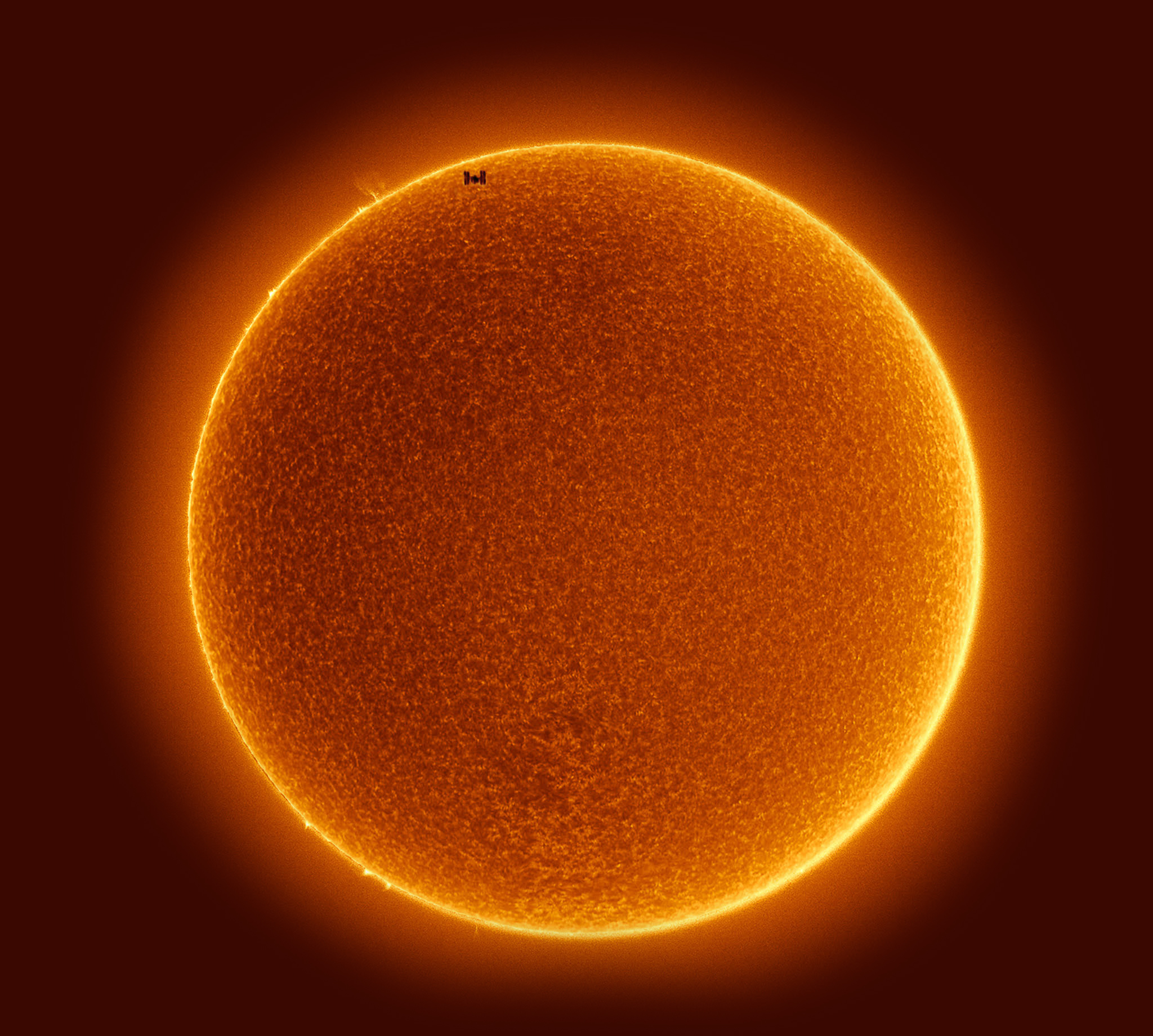
Most basal cell carcinomas are thought to be caused by long-term exposure to ultraviolet (UV) radiation from sunlight. Avoiding the sun and using sunscreen may help protect against basal cell carcinoma.
Symptoms
Basal cell carcinoma usually develops on sun-exposed parts of your body, especially your head and neck. Less often, basal cell carcinoma can develop on parts of your body usually protected from the sun, such as the genitals.
Basal cell carcinoma appears as a change in the skin, such as a growth or a sore that won’t heal. These changes in the skin (lesions) usually have one of the following characteristics:
- A pearly white, skin-colored or pink bump that is translucent, meaning you can see a bit through the surface. Tiny blood vessels are often visible. In people with darker skin tones, the lesion may be darker but still somewhat translucent. The most common type of basal cell carcinoma, this lesion often appears on the face and ears. The lesion may rupture, bleed and scab over.
- A brown, black or blue lesion — or a lesion with dark spots — with a slightly raised, translucent border.
- A flat, scaly, reddish patch with a raised edge is more common on the back or chest. Over time, these patches can grow quite large.
- A white, waxy, scar-like lesion without a clearly defined border, called morpheaform basal cell carcinoma, is the least common.



When to see a doctor?
Make an appointment with your doctor if you observe changes in the appearance of your skin, such as a new growth, a change in a previous growth or a recurring sore.
Dangerous skin problems:
- Basal cell carcinoma
- Actinic keratosis
- Squamous cell carcinoma
- Kaposi-sarcoma
- Melanoma
Causes
Where skin cancer develops
Skin cancer begins in the cells that make up the outer layer (epidermis) of your skin. One type of skin cancer called basal cell carcinoma begins in the basal cells, which make skin cells that continuously push older cells toward the surface. As new cells move upward, they become flattened squamous cells, where a skin cancer called squamous cell carcinoma can occur. Melanoma, another type of skin cancer, arises in the pigment cells (melanocytes).
Basal cell carcinoma occurs when one of the skin’s basal cells develops a mutation in its DNA.
Basal cells are found at the bottom of the epidermis — the outermost layer of skin. Basal cells produce new skin cells. As new skin cells are produced, they push older cells toward the skin’s surface, where the old cells die and are sloughed off.
The process of creating new skin cells is controlled by a basal cell’s DNA. The DNA contains the instructions that tell a cell what to do. The mutation tells the basal cell to multiply rapidly and continue growing when it would normally die. Eventually, the accumulating abnormal cells may form a cancerous tumor — the lesion that appears on the skin.
Ultraviolet light and other causes
Much of the damage to DNA in basal cells is thought to result from ultraviolet (UV) radiation found in sunlight and in commercial tanning lamps and tanning beds. But sun exposure doesn’t explain skin cancers that develop on skin not ordinarily exposed to sunlight. Other factors can contribute to the risk and development of basal cell carcinoma, and the exact cause may in some cases not be clear.
Risk factors
Factors that increase your risk of basal cell carcinoma include:
- Chronic sun exposure. A lot of time spent in the sun — or in commercial tanning beds — increases the risk of basal cell carcinoma. The threat is greater if you live in a sunny or high-altitude location, both of which expose you to more UV radiation. Severe sunburns also increase your risk.
- Radiation therapy. Radiation therapy to treat acne or other skin conditions may increase the risk of basal cell carcinoma at previous treatment sites on the skin.
- Fair skin. The risk of basal cell carcinoma is higher among people who freckle or burn easily or who have very light skin, red or blond hair, or light-colored eyes.
- Increasing age. Because basal cell carcinoma often takes decades to develop, the majority of basal cell carcinomas occur in older adults. But it can also affect younger adults and is becoming more common in people in their 20s and 30s.
- A personal or family history of skin cancer. If you’ve had basal cell carcinoma one or more times, you have a good chance of developing it again. If you have a family history of skin cancer, you may have an increased risk of developing basal cell carcinoma.
- Immune-suppressing drugs. Taking medications that suppress your immune system, such as anti-rejection drugs used after transplant surgery, significantly increases your risk of skin cancer.
- Exposure to arsenic. Arsenic, a toxic metal that’s found widely in the environment, increases the risk of basal cell carcinoma and other cancers. Everyone has some arsenic exposure because it occurs naturally. But some people may have higher exposure if they drink contaminated well water or have a job that involves producing or using arsenic.
- Inherited syndromes that cause skin cancer. Certain rare genetic diseases can increase the risk of basal cell carcinoma, including nevoid basal cell carcinoma syndrome (Gorlin-Goltz syndrome) and xeroderma pigmentosum.


Complications
Complications of basal cell carcinoma can include:
- Risk of recurrence. Basal cell carcinomas commonly recur, even after successful treatment.
- An increased risk of other types of skin cancer. A history of basal cell carcinoma may also increase the chance of developing other types of skin cancer, such as squamous cell carcinoma.
- Cancer that spreads beyond the skin. Very rarely, basal cell carcinoma can spread (metastasize) to nearby lymph nodes and other areas of the body, such as the bones and lungs.
First aid for the skin with the clinically tested plant-based R47-PROTUMOL® treatment cream.
Skin regenerator. Quick and efficient. No side-effects.
Prevention is an investment in the future!
To reduce your risk of basal cell carcinoma you can:
- Avoid the sun during the middle of the day. In many places, the sun’s rays are strongest between about 10 a.m. and 4 p.m. Schedule outdoor activities for other times of the day, even during winter or when the sky is cloudy.
- Wear sunscreen year-round. Use a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply sunscreen generously, and reapply every two hours — or more often if you’re swimming or perspiring.
- Wear protective clothing. Cover your skin with dark, tightly woven clothing that covers your arms and legs, and a broad-brimmed hat, which provides more protection than does a baseball cap or visor. Some companies also sell protective clothing. A dermatologist can recommend an appropriate brand. Don’t forget sunglasses. Look for those that block both types of UV radiation — UVA and UVB rays.
- Avoid tanning beds. Tanning beds emit UV rays and can increase your risk of skin cancer.
- Check your skin regularly and report changes to your doctor. Examine your skin often for new skin growths or changes in existing moles, freckles, bumps and birthmarks. With the help of mirrors, check your face, neck, ears, and scalp.
- Examine your chest and trunk and the tops and undersides of your arms and hands. Examine both the front and the back of your legs and your feet, including the soles and the spaces between your toes. Also, check your genital area and between your buttocks.
- Protect your mole and skin, and use R47-PROTUMOL® cream for prevention.
- Prevention is an investment in the future!
- After each sunbathing and tanning-bed session, apply a thin layer of R47-PROTUMOL® treatment cream on the warts and moles of your body and on the suspicious looking surface skin lesions.
On the one hand it is for prevention because it immediately provides surface skin protection against environmental effects. On the other hand it is also a barrier because with this preventive step you help in blocking the cancerous degeneration of wart and mole cells by means of the natural active ingredients.